Transurethral prostate surgery is a minimally invasive procedure used to treat urinary symptoms caused by benign prostatic hyperplasia (BPH), a noncancerous enlargement of the prostate gland. As the prostate grows, it can press against the urethra and restrict urine flow, leading to symptoms such as difficulty urinating, weak stream, frequent urination, or incomplete bladder emptying. This surgery helps relieve obstruction by removing or reducing the size of the overgrown prostate tissue.
Conditions Treated
- Benign Prostatic Hyperplasia (BPH): The primary indication for transurethral prostate surgery is BPH. The procedure is designed to reduce urinary obstruction and restore normal bladder function.
- Bladder Outlet Obstruction: Caused by an enlarged prostate restricting urine flow through the urethra.
- Recurrent Urinary Tract Infections (UTIs) or Bladder Stones: In some cases, obstruction from BPH can contribute to these secondary issues, and surgery may help prevent recurrence.
Surgical Options
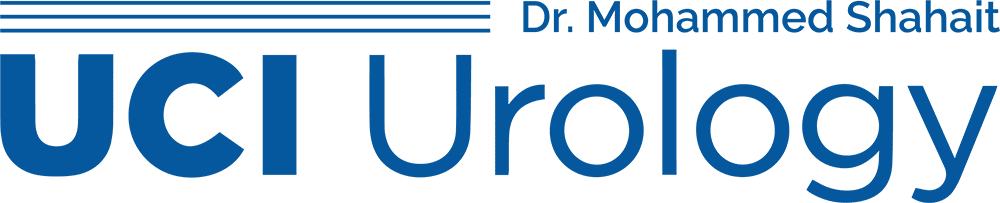
- Transurethral Resection of the Prostate (TURP): The most common approach, TURP involves inserting a resectoscope through the urethra to shave away excess prostate tissue and widen the urinary channel.
- Transurethral Incision of the Prostate (TUIP): In patients with smaller prostates, this procedure involves making one or two small incisions in the prostate to relieve pressure without removing tissue.
- Laser Procedures (e.g., HoLEP, GreenLight PVP): Use laser energy to vaporize or remove prostate tissue with minimal bleeding, often suitable for patients on blood thinners.
- Bipolar Electrosurgery: An advanced variation of TURP using bipolar current, which reduces the risk of complications like TUR syndrome.
What to Expect
- No External Incisions: All procedures are performed through the urethra using specialized instruments.
- Short Hospital Stay: Most patients are discharged the same day or within 24 hours.
- Catheter Use: A urinary catheter is placed temporarily post-surgery to aid healing and ensure bladder drainage.
- Recovery: Most patients resume normal activities within 1–2 weeks, with improved urinary flow often noticeable shortly after catheter removal.
Benefits
- Improved Urinary Flow: Significant relief of obstruction and voiding symptoms.
- Reduced Frequency and Urgency: Many patients experience fewer nighttime trips to the bathroom and less urgency.
- Minimal Invasiveness: No external scars and lower complication rates compared to open surgery.
Next Steps
If you are experiencing persistent urinary symptoms due to BPH, consult a urologist to determine whether transurethral prostate surgery is the right option. A personalized evaluation, including imaging and flow studies, can help guide treatment planning to restore urinary function and improve quality of life.